Traveling while pregnant or breastfeeding brings a whole new layer of complexity. You’re no longer packing just for you—you’re packing for two.
Although pregnancy is a beautiful and natural experience, not a handicap, it alters the body’s physiology, including blood circulation and the immune system.
The embryo and later the fetus are connected to everything that’s happening inside the body; therefore, we need to be extra careful, especially about infections and medication.
Moms often feel what’s best for them and their little ones. But evolution couldn’t prepare us for long-range flights, medication, and vaccines. On the other hand, we now have knowledge about infectious diseases, scientific papers on the use of different drugs, and tools like breast pumps and ultrasound.
This article provides evidence-based travel health information tailored to pregnant and nursing women.
You’ll learn what infections to avoid, what vaccines are safe, and which medications to pack.
In This Article
This post includes affiliate links. If you choose to purchase through these links, I may receive a commission, helping me continue creating valuable content for you. This comes at no additional cost to you.
We receive a fee when you get a quote from World Nomads using links in this post. We do not represent World Nomads. This is not a recommendation to buy travel insurance.
Is It Safe to Travel While Pregnant or Breastfeeding?
Yes—if you’re careful.
Most healthy pregnant women can travel safely, and the second trimester is considered the safest window. The risk of miscarriage has dropped, and you’re still mobile and (hopefully) not too uncomfortable.
In your third trimester, the risk of complications such as bleeding, preterm labor, or preeclampsia rises, and some airlines won’t allow you on board after the 35th week.
Breastfeeding travelers face fewer physiological risks but still need to plan around milk storage, feeding schedules, and medication safety.
Always consult your OB-GYN before booking tickets, especially if you have high-risk conditions like multiple gestations or clotting disorders.

Flying While Pregnant or Breastfeeding: What to Know
Flying is generally safe.
Your baby won’t suffer from a lack of oxygen at altitude thanks to the fetal hemoglobin curve (the fetal blood can bind oxygen “stronger” than the mother’s, making it fully saturated even when the mother’s oxygen levels are slightly lower).
Maybe you’ve heard about cosmic radiation during air travel. In general, the fetus is most sensitive to radiation in the 8th to 14th weeks of gestation. So, should you avoid flying because of this?
In pregnancy, exposure to 1 milliSievert (mSv) is considered safe for the baby. The dose you get on a flight differs based on altitude and latitude, but on average, it is 0.004 mSv per hour. That means you’d have to fly for 250 hours to cross the limit. That’s 24 flights from LA to London.
And what about airport full-body scanners? Nowadays, most airports use so-called millimeter wave scanners, which use radio waves. If they still use X-rays, the whole body screen will give you a “staggering” 0.00001 mSv of ionizing radiation. That’s 10 times less radiation than what eating a banana gives you. Yes, bananas contain potassium, and a small fraction of it is radioactive.
The point is that the amount of radiation is negligible for an average traveler.

A real threat of air travel (not only) during pregnancy is blood clots.
Pregnancy raises the risk, and sitting still at 35,000 feet doesn’t help.
Choose an aisle seat, wear compression stockings, and walk around regularly. You should never take aspirin, but you may consult your physician about other blood thinners if you’re at high risk.
Remember, the risk of thrombosis remains high at least 6 weeks after delivery.
If you’re breastfeeding, good news: Milk, formula, and breast pumps have plenty of exemptions when going through security.
Stay hydrated on the flight and breastfeed during takeoff and landing to help your baby’s middle ear pressure equalize.
Food and Water Safety While Traveling
Your biggest enemies abroad? Not spicy food or airplane meals—traveler’s diarrhea, Listeria, and hepatitis E.
Pregnant women are more vulnerable to dehydration and infections. Listeria, found in unpasteurized dairy and deli meats, can cause miscarriage or stillbirth. Skip soft cheeses like Brie and Feta, and say no to cold cuts.
Avoid tap water in high-risk regions. Stick to bottled, boiled, or filtered water using virus-removing filters. Don’t use iodine tablets for chemical water purification. Skip street food unless it’s piping hot.
If diarrhea hits, oral rehydration salts (ORS) are safe to use. From the medication, loperamide (e.g., Immodium®) may be used cautiously, and Azithromycin is the safest antibiotic if needed.
Avoid Pepto-Bismol® (bismuth)—it’s not safe in pregnancy or lactation.
High Altitude Travel: Worth the Risk?
Heading to Cusco or Kilimanjaro? Think twice.
Pregnant travelers should avoid elevations above 3,000 meters.
Although there are limited data, high altitude may pose a risk of fetal growth restriction and preeclampsia.
Short trips with gradual ascent may be safe, but physical activities in high altitudes should be avoided.
Acetazolamide is not recommended in pregnancy and should be avoided during lactation if possible. Focus on prevention—take it slow, and don’t exert yourself. Read more about high altitude here.
Vaccines: What’s Safe, What’s Not
Inactivated vaccines like Tdap, flu, or RSV may be recommended in pregnancy, whether you travel or not.
Other non-live vaccines, such as hepatitis A/B, Rabies, or Typhoid fever, are generally safe, but a physician must individually assess them based on the travel risk.
Live vaccines like MMR and varicella are generally contraindicated in pregnancy.
Women should postpone conception at least 4 weeks after administering a live vaccine. However, if given by accident, don’t panic—there’s no proven fetal harm, and termination is not advised.

The yellow fever vaccine?
It’s tricky. It’s live but may be given if travel to an endemic area is unavoidable. Some studies show no harm, but weigh the risks carefully.
A medical waiver should be obtained if the vaccination is required at the border, but there’s no risk for the traveler.
If the yellow fever vaccine has been given in pregnancy, one more dose should be given later in life to ensure lifelong protection.
For breastfeeding moms, the yellow fever vaccine should be avoided unless absolutely necessary—there have been cases of neonatal encephalitis in the breastfed infants.
If vaccinated, consider pumping and discarding milk for 2 weeks. Non-live vaccines can be used safely.
Infections to Avoid in the Tropics
If you’re pregnant, avoid mosquito-borne illnesses like the plague. Infectious diseases like Malaria, Zika, Dengue, and others have worse outcomes in pregnancy for both the mother and the fetus.
If you live in areas where these illnesses are not present, it’s advised to avoid traveling to such destinations during pregnancy and with a newborn.
Zika
It’s a confirmed teratogen (agent causing developmental abnormalities) linked to microcephaly, eye defects, and brain damage. Currently, there’s no vaccine.
Avoid areas with active Zika transmission.
And don’t forget: Zika can be sexually transmitted—so your partner’s travel matters too.
The virus has been found in semen for up to 6 months after infection. That’s why couples traveling to areas with Zika transmission should postpone conception for at least 6 months.
– countries with Zika transmission (CDC)
Dengue & Chikungunya
Linked to miscarriage, low birth weight, and neonatal complications. Reconsider travel to affected regions. These aren’t passed through breast milk. Read more about Dengue here.
– areas with risk of Dengue (CDC)
– areas at risk for Chikungunya (CDC)
Oropouche
This lesser-known virus is spreading fast in parts of South America. The CDC recommends that pregnant women avoid non-essential travel to outbreak zones.
– current outbreak zones (CDC)
If traveling is unavoidable, avoid mosquito bites using EPA-approved repellents like DEET and picaridin. They’re safe in pregnancy and while breastfeeding.

Malaria: Why It’s So Dangerous in Pregnancy
This one’s a deal-breaker.
Pregnant women are more likely to get severe malaria, which can lead to miscarriage, stillbirth, and maternal death.
If possible, do not travel to high-risk areas, especially those with high falciparum Malaria (sub-Saharan Africa). Other malaria parasites, such as P. vivax, which are more common in Latin America or parts of Asia, may be less dangerous, but still have negative consequences for the mother and newborn.
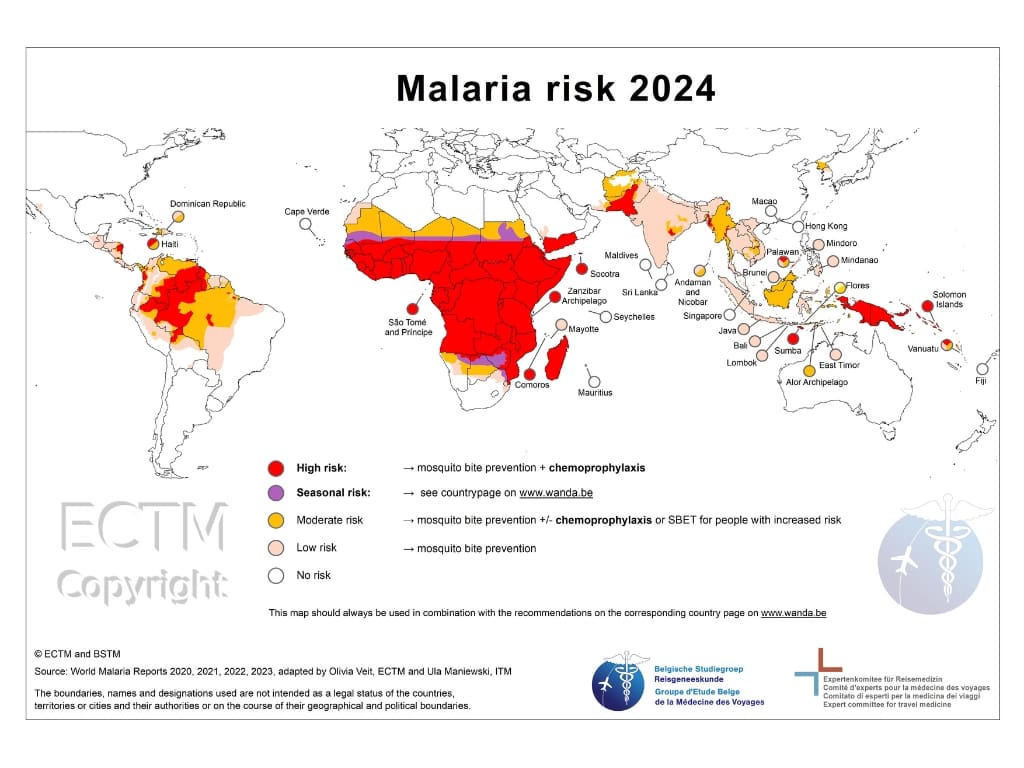
If you must go, use mosquito nets, repellents, and prophylaxis (malaria prevention medicine).
Chloroquine (Plaquenil®) is safe to take in pregnancy, but P. falciparum is resistant to it almost worldwide.
Mefloquine (Lariam®) can be taken in all trimesters, if necessary. Although not specifically approved for pregnancy, limited data suggest it’s safe and certainly a better choice than risking getting malaria, and medicine for malaria treatment.
Atovaquone-proguanil (MalaroneTM) is not advised in the first trimester and should be used cautiously in breastfeeding (only if the baby is 5kg+). Both mefloquine and chloroquine can be used while breastfeeding.
No primaquine or tafenoquine during pregnancy, or if your nursing baby hasn’t been tested for G6PD enzyme deficiency.
Safe Medications for Travel
You’ll want to travel light—but not when it comes to your meds. In pregnancy, we have to think twice before taking any medication.
For most, there is very little data about whether they can cause harm to the baby or not.
May be used safely:
- Acetaminophen for pain/fever
- ORS packets for dehydration
- Dimenhydrinate or meclizine for motion sickness
- Loperamide and Azithromycin for moderate and severe traveler’s diarrhea (cautiously, and only when the benefit outweighs the risk)
Always avoid:
- NSAIDs – Ibuprofen (Motrin®, Advil®), Naproxen sodium (Aleve®) (especially in the 3rd trimester)
- Aspirin
- Bismuth subsalicylate (Pepto-Bismol)
- Doxycycline (used for malaria prophylaxis)
- Iodine (for water purification)

Ask your physician about any new medication while pregnant or breastfeeding.
You can check these resources for medication in pregnancy, and while breastfeeding:
Essentials to Pack: Medical Kit for Two
You’re not just packing sunscreen.
Must-haves:
- Prenatal vitamins
- DEET or picaridin repellent
- Ginger chews or wristbands (for nausea)
- Breast pump & milk storage bags
- Prescribed meds + letter from your doctor
For high-risk moms:
- Sphygmomanometer (for measuring blood pressure)
- Urine dipsticks (to check proteins in urine)
Bonus tip: Check your travel insurance—not all plans cover delivery abroad.
Final Thoughts: Plan Smart, Travel Safe
Traveling while pregnant or breastfeeding isn’t impossible, but it does require strategy.
- Avoid risky regions; it’s not worth it
- Use safe vaccines and medications if needed
- Pack the important stuff to handle emergencies
- Consult your doctor or travel medicine specialist for guidance
You’ve got this!
Want more tips like this?
Follow me on Instagram, subscribe to my newsletter, and share this with someone planning their babymoon.
Resources
Centers for Disease Control and Prevention (CDC). (2025). CDC Yellow Book 2026: Health Information for International Travel. Oxford University Press.
Travel Medicine, 4th Edition – December 13, 2018, Authors: Jay S. Keystone, Phyllis E. Kozarsky, Bradley A. Connor, Hans D. Nothdurft, Marc Mendelson, Karin Leder, Language: English, Hardback ISBN: 9780323546966
AAPM Report No. 217 Radiation Dose from Airport Scanners”. American Association of Physicists in Medicine. June 2013. Retrieved 30 June 2025.
Friedberg, W; Copeland K (2011). “Ionizing Radiation in Earth’s Atmosphere and in Space Near Earth” Civil Aerospace Medical Institute, Federal Aviation Administration, DOT/FAA/AM- 11/9.
Disclaimer:
The information provided in this blog post is for general informational and educational purposes only and is not a substitute for professional medical advice. Always consult your physician or other qualified healthcare provider with any health problem. The use or reliance on any information provided in this blog post is solely at your own risk.